CURRICULUM
-
Cardiac Care Unit (CCU): The CCU experience provides in-depth training in advanced cardiac pathology and critical care medicine. Fellows round in the 18-bed CCU with internal medicine residents, students, and dedicated pharmacists. Furthermore, fellows follow post-operative cardiac surgery patients in the cardiothoracic surgical ICU (CPS). Fellows are involved in the management of mechanical support devices (intra-aortic balloon pump, Impella, ECMO). Lastly, fellows perform consults in non-cardiac intensive care units including the medical ICU (MICU), surgical ICU (SICU), and neurosciences ICU, providing a broad exposure to critical care medicine. In particular, the cardiac ICU service works closely with our pulmonary/critical-care medicine colleagues who remain in-house 24 hours daily.
-
Cardiac Catheterization: The cardiac catherization rotation involves all aspects of diagnostic and interventional angiography, along with structural heart interventions. Fellows develop graded responsibility, and often independently perform diagnostic angiograms with attending supervision by their third year of fellowship. Pre and post cath patient management, case selection for interventional or surgical treatment for coronary disease, fundamentals of access and coronary interventions, hemodynamics and percutaneous ventricular support devices are some of the topics covered during the cardiology training program. Aside from the clinical work, fellows participate and lead weekly interventional and hemodynamic conferences and didactic lectures. AMC routinely performs the latest structural inventions, including TAVR procedures, MitraClip percutaneous mitral valve repair, and left atrial appendage occlusion (Watchman procedure).
-
Didactic Curriculum: To facilitate independent and Faculty supervised learning, we offer a comprehensive structured didactic program which covers all areas of cardiovascular medicine as required by COCATs training curriculum and ABIM Board certification.
Each academic year, there are 12 learning modules with clearly defined learning objectives coupled to the reading material, post-reading self-assessment, didactic lectures, interactive clinical case discussions, and hands-on sessions.
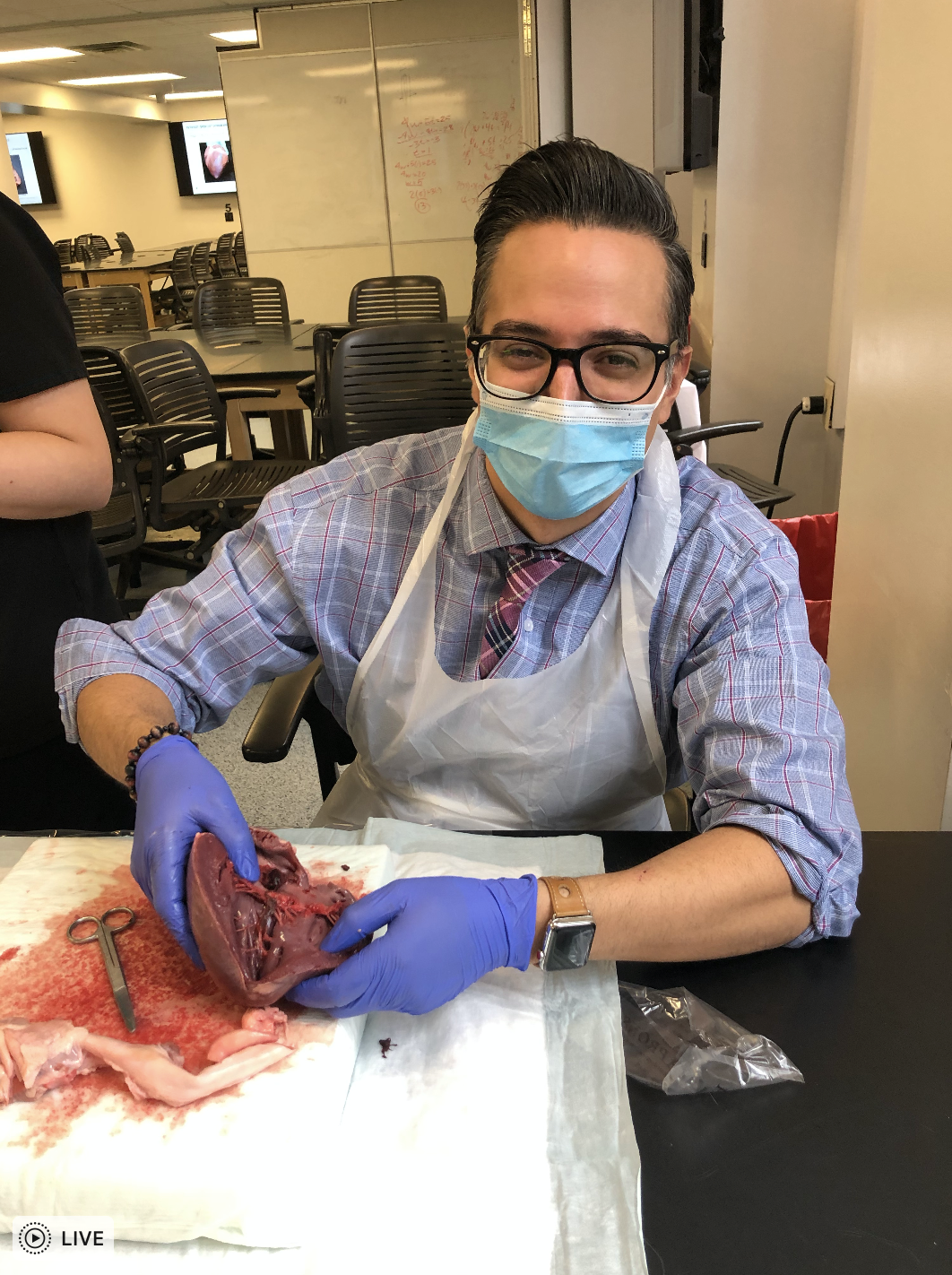
Individual learning sessions are run by the Fellowship Faculty and also by the invited faculty experts in Cardiac Surgery, Vascular Surgery, Endocrinology, Pulmonary Medicine, Pathology, Clinical Nutrition, and other disciplines relevant to cardiovascular medicine. The hands-on sessions include heart dissection, transesophageal echocardiography simulation, management of cardiac assist devices, and pacemaker-ICD interrogation tutorials.
The program is tailored to the fellow level of training, progressing from the foundation of the Cardiovascular medicine to advanced complex material consistent with modern cardiovascular medicine practice expectations.
We strive to encourage active fellow participation and advocate interactive learning based on the relevant clinical material.
Fellows are also expected to participate in cardiovascular research training which includes journal club discussions of basic research tools and carrying out a supervised investigative project. A wide variety of subjects are studied, ranging from preventative cardiology to advanced structural heart disease interventions. Fellow initiated projects are encouraged, with ample opportunities to participate in multi-center trials and registries.
-
Elective: Third year fellows may request elective time in pediatric/congenital cardiology, cardio-oncology, or vascular ultrasound. In addition, fellows are encouraged to spend time in AMC radiology for cardiac CT and cardiac MRI (CMR) experience outside of dedicated elective time. Cardiac CT and CMR have become routine complementary modalities at AMC.
-
Electrophysiology (EP): The EP rotation for fellows is a combination of inpatient consultation, outpatient clinic visits, and procedures in the EP lab. Routine EP procedures performed at AMC includediagnostic electrophysiology studies, supraventricular tachycardia ablation, typical atrial flutter ablation, pacemaker and defibrillator implants, loop recorder implants, lead extraction, and complex ablations. Fellows will become familiar with complex ablations for atrial fibrillation, atypical atrial flutter, PVCs, and ventricular tachycardia. The EP consult service provides fellows with an opportunity to learnmanagement of patients with a variety of arrhythmias and implanted devices through one-on-one rounding with an EP attending, thereby assisting the CCU and general cardiology teams.
-
Heart Failure (HF): The heart failure faculty consists of two fellowship-trained heart failure/transplant cardiologists who practice in collaboration with a multidisciplinary care team. The clinical experience for cardiovascular medicine fellows emphasizes consultative care of patients with heart failure and cardiomyopathy as well as those who are candidates for, or have previously undergone, heart transplantation or mechanical circulatory support. We offer special exposure to the evaluation of patients presenting with cardiomyopathy using various diagnostic tools including imaging methods, endomyocardial biopsy, and genetic testing. There is a balance of inpatient and outpatient activities, and the fellow will typically attend 4 specialized heart failure outpatient clinic sessions per week. The didactic component of the heart failure rotation is robust; a substantial portion of our fellowship’s unique self-study curriculum (described elsewhere) is devoted to advanced heart failure, cardiomyopathy, and heart transplantation. Over the last few years, fully 25% of our graduating fellows have pursued advanced training in heart failure and transplantation, successfully matching in HF programs including the University of Rochester, Montefiore Medical Center, Virginia Commonwealth University, and the University of Chicago.
-
Inpatient/Consultation Service: This service provides the core of non-ICU clinical cardiology training. Fellows and attending cardiologists are responsible for managing a primary service of cardiac patients, as well as consulting on patients across the hospital admitted under all other services. A strong hospitalist program at Albany Medical Center allows for co-management of complex patients under the internal medicine service. Fellows are responsible for consults requested by the Emergency Department. Lastly, fellows on this rotation work closely with all other fellows on subspecialty rotations to provide the highest-level team-based care.
-
Night Float: The night float system affords fellows the opportunity to participate in core and elective rotations without the interruption of call shifts during the week. The night float fellow works 5 overnight shifts a week, for a total of 2 weeks at a time. Fellows are generally scheduled on the night float rotation once every academic half-year. This rotation prepares the cardiology fellow for autonomous clinical management, while also offering an invaluable consultative experience. Further, night float ensures an uninterrupted, in-house cardiology presence for our patients.
-
Non-invasive Cardiology (NIC)/Echocardiography: The AMC Cardiology department is well-known in part due to the strength of its echocardiographic laboratory. On this rotation fellows learn to master the art of echocardiographic interpretation, after learning to scan with the echo techs. To facilitate training in echocardiography, our faculty has developed an interactive iBook https://books.apple.com/us/book/i-read-echos/id576192519 which presents a comprehensive approach to echocardiography and interpretation of an adult transthoracic echocardiogram. Unlike standard textbooks, this iBook is organized accordingly to the standard image/view acquisition sequence, which is the way the echocardiographic images are presented and interpreted.
Fellows are also responsible for performing and interpreting trans-esophageal echocardiograms (TEEs), after evaluating appropriateness of patients for such procedures. Fellows will also learn advanced echocardiographic techniques such as exercise and Dobutamine stress echocardiography, viability studies, strain and 3D imaging. Lastly, fellows perform exercise and Lexiscan nuclear myocardial perfusion imaging, and learn to interpret ECGs and imaging with board-certified cardiologists and radiologists.
-
Research: A minimum of 4 weeks per year of dedicated research elective time is given to each fellow yearly to pursue either clinical research or quality improvement projects. All fellows are expected to complete their own research/scholarly project with attending guidance and mentorship by the end of fellowship and submit their scholarly work as both an abstract and manuscript to regional or national conferences and peer reviewed journals respectively. AMC has access to national AHA GWTG Heart Failure and Mission Lifeline STEMI databases.
-
VA Cardiology Service: The Stratton VAMC provides fellows with a unique clinical experience serving Capital Region veterans from a large geographical area extending from the Canadian border to the southern tier and into western Massachusetts and SW Vermont. This is a multi-modality service involving outpatient clinic experience, inpatient consultation, invasive and device procedures, ECG interpretation, cardioversions and trans-esophageal echocardiography. There are growing opportunities to participate in virtual care delivery. Two fellows are assigned to the VAMC at any given time.






AMC Cardiology Fellows & Attendings
Spring 2018


